“Just having a safe space for somebody to enter into and have a conversation as well as get their basic needs met is so essential for relationship building.”
Andrew Volkers (he/they), COVID-19 Mitigation Coordinator
Andrew Volkers works at the Maine Medical Center-Preble Street Learning Collaborative, the Learning Collaborative for short, which provides low-barrier healthcare, care coordination services, and health education to unsheltered Mainers.
Maine Medical Center, Preble Street, and other community partners established the Learning Collaborative in January 2017 to bridge the well documented gap between the unsheltered population and healthcare services. People experiencing homelessness face devastating physical and mental outcomes and seemingly insurmountable barriers to accessing healthcare and treatment. The U.S. Department of Housing and Urban Development reported that people experiencing homeless are more than twice as likely to have a disability than the general population, and, in 2023, HUD reported unsheltered individuals also experience chronic and mental illness at significantly higher rates than the general public: 31 percent reported having a serious mental illness on a given night and 24 percent reported conditions related to chronic substance use.
On a given night in 2023...
Continue reading here for HUD’s 2023 Point in Time data.
Treatment and preventative care are less accessible to people experiencing homelessness for many reasons, but one of the biggest barriers is cost and lack of insurance. Many communities now have Federally Qualified Health Centers (FQHC) – Preble Street’s Recuperative Care (RCP) is part of a Federally Qualified Health Center facility – that provide basic services for little or no cost. The Affordable Care Act has also enabled states to expand Medicaid programs to provide healthcare coverage to people with lower incomes. Although access to healthcare in Maine has expanded through Maine Care, and there are 144 FQHCs throughout the state, many barriers, like transportation, prejudice against homelessness, etc., still persist and block access to care.
The Learning Collaborative identifies these roadblocks to care and emphasizes building rapport and trust with people experiencing homelessness.
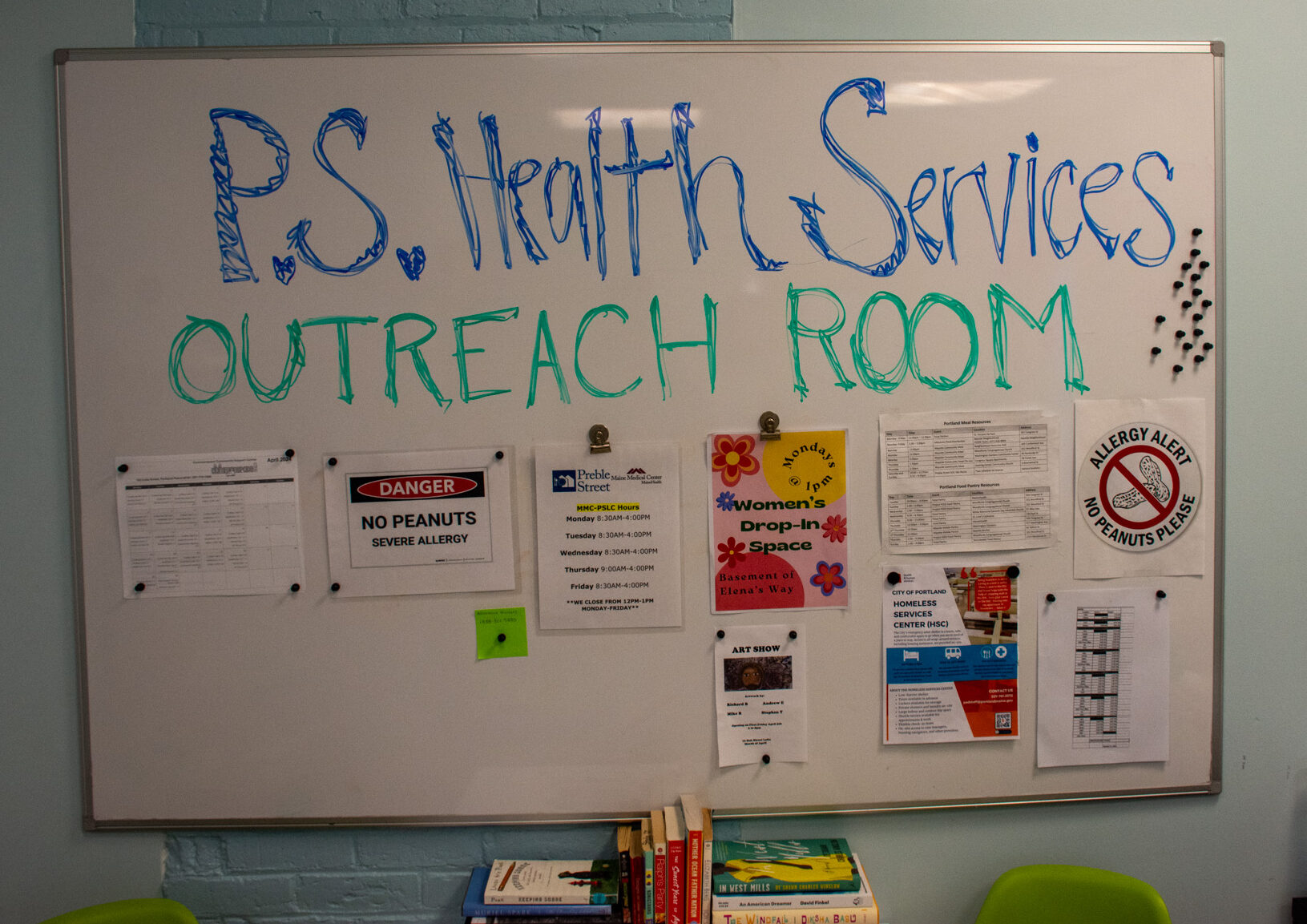
This starts in the Outreach Room…
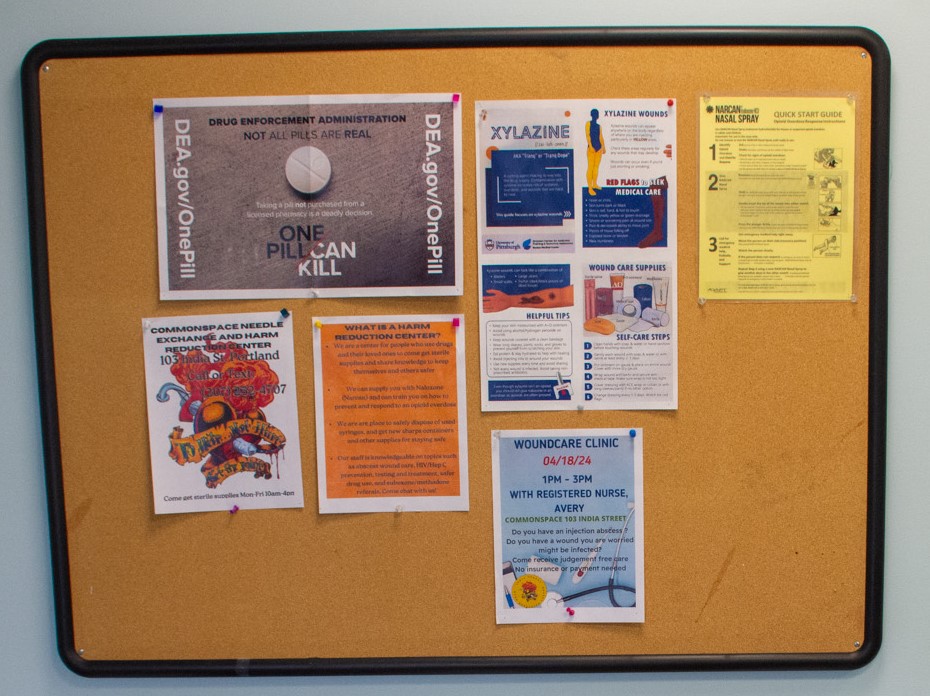
The Outreach Room is the first point of contact for people who come in seeking treatment, care coordination, or just help with basic needs. “When people come in, we can offer them food, socks, toiletries, harm reduction supplies, or just have casual conversations,” says Andrew. Meeting people where they’re at with basic needs, like toiletries, a snack, or a casual conversation becomes the basis and entry into long-term healthcare and care coordination: “People will come in and grab harm reduction supplies or a toothbrush. Then, they’ll keep coming back and that relationship will grow to the point where I can ask ‘Hey, are you ready to see the doctor? Hey, are you ready to go to the shelter tonight?’”
Caroline Fernandes (she/her), Health Services Director at the Learning Collaborative, adds, “We have folks here that would never go in and see the Doctor. Now, they’re getting comprehensive medical care – staying at the hospital or having care here at the Learning Collaborative.”
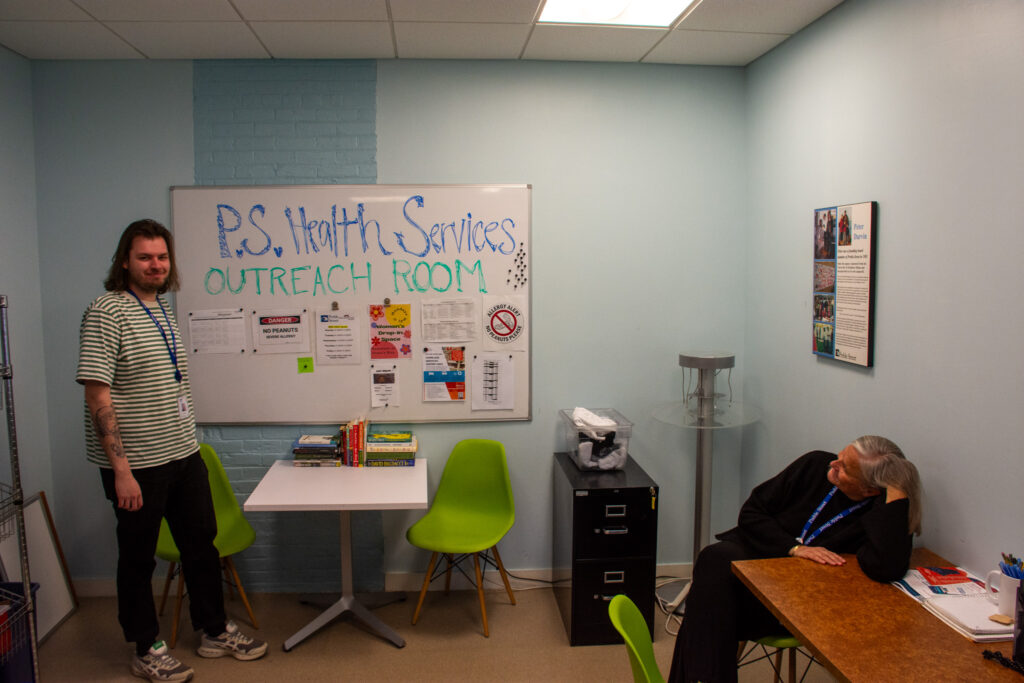
Andrew and Caroline pictured in the Outreach Room.

Some of the basic needs items, like toiletries and harm reduction supplies, seen in the Outreach Room.
People can receive care from an onsite Maine Medical Center health care provider, who can perform clinical services, including triage as well as urgent, follow-up, and wound care.
MMC’s Homeless HealthPartners (HHP) case management team is also co-located at the Learning Collaborative site, working alongside Preble Street and health provides to provide short-term case management and coordinating access to primary care and other medical providers.
Alongside the various barriers to entry, many people experiencing homelessness have had negative experiences with the healthcare system or are simply worried about cost. “Many, for the first time, go to the emergency department or get major medical issues addressed because of the relationships they develop in this space,” Caroline explains.
The Learning Collaborative’s Outreach Room is also a place where people can learn about community events and resources. “We want to have a lot of resources for people in the community, like where you can get food 24/7, where you can get Narcan in the middle of the night, and what are different activities in the community,” says Caroline.
The Outreach Room previously emphasized basic needs above all else – clothes, toiletries, harm reduction supplies, etc. – in the wake of the various encampment sweeps and swelling need in Portland. Now, Andrew and Caroline are transitioning this space to follow a comprehensive outreach model, still providing basic needs but using that as an entry to connecting people to other resources, like medical services, shelter, SNAP benefits, community events, and more. Posters hang on the wall, advertising a community grief group, a woman’s drop-in group, and a community art show organized by Learning Collaborative clients.
Community resources and posters seen in the Outreach Room.
The Learning Collaborative was created in part to reduce stigma among medical providers in Maine and for providers to receive hands-on experience, working with the unsheltered population and thus preparing them to become better providers to all people regardless of their health or situation. In fact, many people who do a rotation at the Learning Collaborative go on to work there full time or spend additional time with patients. As the name suggests, it is a place of continual learning, with patients and providers learning from each other and the larger healthcare system learning from its model of care.
The Learning Collaborative is located at 20 Portland Street, Portland Maine 04102.

Social work is at the heart of the MaineHealth-Preble Street Learning Collaborative
People who are homeless experience severe physical and mental health outcomes, facing many barriers to accessing healthcare and treatment. These barriers can include things like the high cost of care, a lack of insurance, distance or transportation, and even prejudice from the medical community. The MaineHealth-Preble Street Learning Collaborative (MH-PSLC) is a low-barrier, walk-in medical clinic in

Preble Street’s Recuperative Care is a one-of-a-kind program for Maine
Art, books, and inspiring messages are found inside and on the walls at Maine’s first recuperative care program. Picture this… you’ve endured a difficult surgery or have had a life-threatening illness or injury. You’re about to embark on a long recovery process, and will soon be discharged from the hospital and have nowhere to go

MaineHealth CONNECT Van started service on July 1
National data from Harvard Medical School show that mobile health clinics are money savers that connect people to preventative care and outpatient services. Across the country, mobile clinics have reduced emergency department visits, returned money to communities, and saved lives. On July 1, MaineHealth launched their very own mobile health clinic, called the CONNECT Outreach Van. The CONNECT